Renal Artery Duplex Demystified: Scan Smarter, Not Harder - Tips, Tricks & then some
Renal artery duplex exams are like the Goldilocks of vascular ultrasound—everything needs to be just right. Too much bowel gas? No image. Too much patient movement? Velocity waveforms wave goodbye. Too little angle correction? Well… good luck defending that PSV on your worksheet. But when done correctly, renal duplex can be one of the most rewarding (and diagnostic) vascular studies we perform.
✅Why Renal Artery Duplex Matters
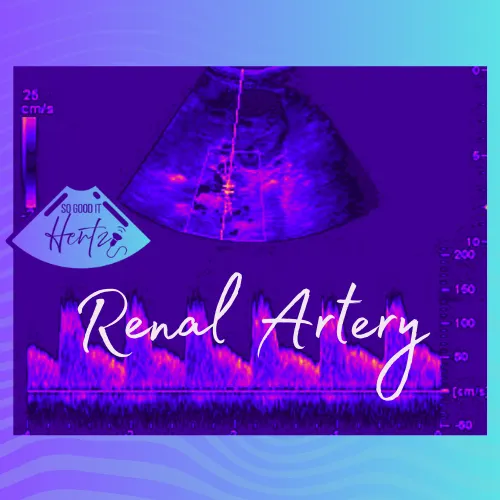
Renal artery stenosis is a leading cause of secondary hypertension and, left unchecked, can have a major impact on renal function. Duplex ultrasound allows us to non-invasively evaluate for narrowing, assess hemodynamics, and help determine whether intervention may be needed. Done well, it can spare patients invasive angiography—or at least guide it more effectively.
And let’s be honest: who doesn’t enjoy chasing renal arteries that like to hide behind every bit of bowel gas in the abdomen? It’s basically the sonographer’s version of hide-and-seek.
✅Patient Prep and Positioning
Tip number one: hydrate your patient before the exam… but not too much. A full bladder is not your friend here. Fasting is best, as reduced bowel gas = reduced sonographer frustration.
Positioning-wise, remember that left lateral decubitus can be your best ally when bowel gas becomes enemy #1. And sometimes, a little “deep breath and hold” maneuver is all it takes to bring the renal artery out of hiding.
Pro Tip: If your patient cannot follow breath-holding instructions, don’t panic. Adjust your window. Sometimes rolling them into a semi-oblique position or using a lower intercostal approach saves the day.
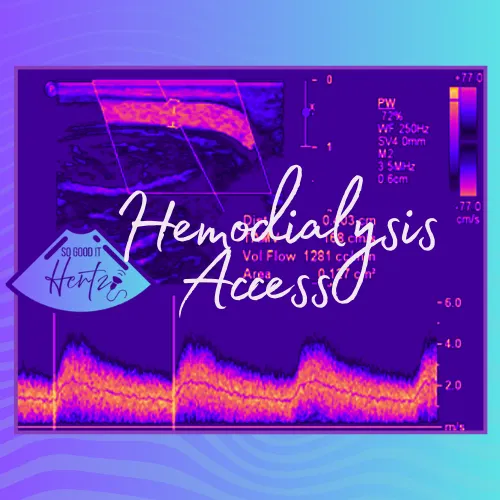
✅Technical Pearls and PSV Pitfalls
- Angle correction is king. Keep it under 60°, and align carefully with flow. That “I’ll fix it later” approach will come back to haunt you in velocity interpretation.
- Sample systematically. Start at the origin, sweep through proximal, mid, and distal segments, and don’t forget to check accessory arteries if you suspect them. (Yes, they’re real, and yes, they love to complicate your life.)
- Don’t trust numbers blindly. PSV >200 cm/s is suspicious, but context matters. Always consider renal-aortic ratio (RAR) and waveform morphology.
Humor moment: If you get an abnormal renal to aortic ratio at the renal origin but your aortic PSV is 65 cm/s, congratulations—you may have just discovered “The Sonographer’s Mirage.” Always check the aortic baseline PSV for accuracy when comparing with a renal to aortic ratio.
Remember, the PSV in the renal artery is compared to the PSV in the aorta. This ratio helps normalize the measurements, accounting for the patient's overall cardiac output and blood flow. However, with very low cardiac output, the baseline aortic PSV is abnormally low, leading to a misleadingly high renal-to-aortic ratio (RAR). remember these key parameters:
Renal-to-Aortic Ratio (RAR):
- A normal RAR is typically below 3.5
- An RAR greater than 3.5 suggests a clinically significant stenosis (generally >60%)
✅When in Doubt, Think Indirect
Sometimes the renal arteries just won’t cooperate. That’s when segmental waveforms come into play. Look for tardus-parvus patterns in the intrarenal vessels—low acceleration, rounded systolic upstroke—that whisper “proximal stenosis” without you ever seeing the lesion.
The Takeaway 🎯
Renal artery duplex is equal parts art and science. It demands patience, technique, and a healthy sense of humor when bowel gas and noncompliant patients test your willpower. Remember: optimize your window, respect your angle correction, and never hang your hat on a single velocity without context.
And above all—when in doubt, scan it out.
-Lara Williams, BS, ACS, RCCS, RDCS, RVT, RDMS, FASE
Don't forget to check out the other platforms below and click that LEARN button up top to check out All About Ultrasound for access to FREE CME!
YouTube: https://www.youtube.com/@SonographersAfterDark
TikTok: https://www.tiktok.com/@sonographersafterdark
Facebook: https://www.facebook.com/groups/sonographersafterdark
Instagram: https://www.instagram.com/sonographersafterdark/